Transarterial chemoembolisation (TACE)
Dear reader, dear patient,
On the following pages we would like to inform you about the Trans-Arterial percutaneous Chemo-Embolisation (TACE) offered at our institution.
There are various forms of curative therapy available for the treatment of liver tumors. Among these are methods like Laser- Induced Thermotherapy (LITT) which is regularly performed at our institution, and other special local treatment methods ( e.g., alcohol instillation) in addition to surgical resection. Various systemic medications (chemotherapy) are used along with these procedures. "Transarterial Chemoembolization (TACE)" which is performed on a regular basis at our institution shows promising results in the treatment of liver metastases. The choice of therapy, combination of different medications and also the time of starting the therapy have not been standardized and are adapted to the individual patient requirements. In TACE, the knowledge of difference in blood supply to the tumor and liver tissue is used. Up to 75% of the normal liver tissue is perfused by the portal venous system and only 25% is supplied by arteries. On the contrary, liver tumors are supplied up to 95% by arteries. Hence chemoembolization of liver arteries lead to development of ischemic necrosis in the tumor region while the remaining normal liver tissue is spared by sufficient perfusion through the portal venous system.
Above all, application of chemotherapy through the major arteries into the liver arteries allows one to achieve a concentration 100 times higher than by systemic approach with only minimal adverse effects. The half-life of chemotherapeutic agent is increased by hours to weeks through the stoppage of blood supply.
Patients' reports after their TACE
Indications
Indications for Transarterial Chemoembolisation:
- Unresectable (surgically or by laser induced thermotherapy) liver metastases and primary Livertumors diagnosed intraoperatively or morphologically using CT and MRI examinations.
- Not responding to systemic chemotherapy.
Criteria for transarterial chemoembolization:
Pre-conditions for Trans-Arterial Chemo-Embolisation:
- Normal liver vessel architecture with good perfusion of both liver lobes.
- Patent portal vein.
- No ascites.
- Good liver function.
- Good general condition of the patient.
Advantages of Trans-Arterial Chemoembolization:
The Trans-Arterial Chemo-Embolisation:
- Associated with very little stress for the patient
- Complication-free Procedure with good quality of life
- Relatively shortened hospital stay (done on an outpatient basis)
- Reduction of tumour growth or reduction in tumour size
Patient with hepatocellular carcinoma (HCC).

The CT image taken after 24 hours of intervention shows a good emplacement of the chemoembolisat.
Principle
The therapeutic procedure of TACE is based on the selective regional application of a chemotherapeutic substance with subsequent occlusion. Therefore, the cytostatic concentration within a tumour and the arterial hypervascularisation of the tumour are the decisive parameters that define the extent of tumour destruction.
of the tumour are the decisive parameters that define the extent of tumour destruction. In addition, the combination of chemotherapy and ischaemia within the tumour allows synergistic effects to achieve maximum tumour necrosis. Using TACE, a high dose of the chemotherapeutic agent is delivered specifically to the tumour cells, prolonging the contact time between the cytostatic drugs and the tumour cells. This also reduces the extent
of embolisation is an important parameter. The healthy liver parenchyma will be spared in the process.
Technology
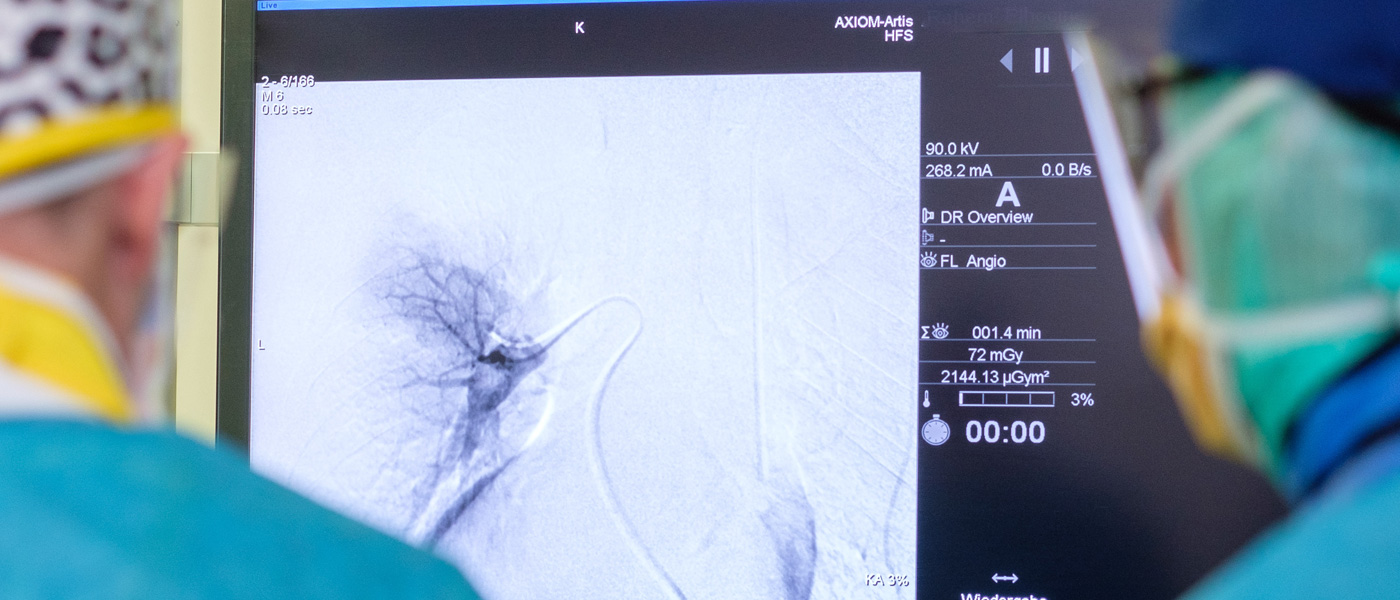
Prior to chemoembolisation treatment, patients should observe a food abstinence of 6 h, although clear liquids or necessary medication can be taken up to 2 h before the procedure. To reduce acute discomfort in the form of upper abdominal pain or nausea during TACE, the patient is administered an opioid and, if necessary, glucocorticoids in a standardised manner via an intravenous line. Before the treatment, all patients are informed about side effects and the risks of the procedure. The main concern is the possibility of embolisation syndrome, which can occur in varying degrees in 5-50% of all TACE procedures. The embolisation syndrome has different effects such as pain symptoms, fever, nausea and vomiting and can last from a few hours to a few days. During angiographic intervention, a pigtail catheter is used for primary visualisation of the abdominal aorta. The coeliac trunk and the superior mesenteric artery are probed with a cobra or sidewinder catheter.
probes. All tumour-supplying arteries and their possible collaterals are visualised and indirect splenoportography is performed via the superior mesenteric and/or lienal arteries.
lienal artery. These angiographic series are intended to show the normal variants of the vessels supplying the liver and to detect the presence of an arteriovenous or arterioportal shunt.
arterioportal shunts as well as a partial or complete thrombosis of the vena portae. For the localisation of the tumour, the early arterial and late venous phases are taken from the angiographic series.
phases are evaluated from the angiographic series. Depending on tumour size, localisation and vascular topography, the selective/superselective placement of the catheter is then
is performed. Due to the risk of vasospasm, it is recommended to use a microcatheter (2.3-3 F) that is positioned superselectively in the regional segmental arteries using a coaxial technique.
segmental arteries using a coaxial technique. The embolisation emulsion is applied under pulsed fluoroscopy. Reflux into the lienal artery, the sinistral gastric artery and the gastroduodenal artery must be prevented.
gastroduodenal and cystic arteries must be prevented. Comparative studies show that the survival rates after TACE for patients with vascular anomalies that can be intervened with
vascular anomalies and collateral circulation are comparable to those with normal topographical conditions.
Intervention
Before the treatment a good visualisation and likewise localisation of the tumor is made with the help of our modern digital imaging machines like the MRI or CT so that the embolisat can be injected exactly in the tumour tissue.

After local anesthesia, a puncture is made into the femoral artery in the inguinal region. Doing this, a small femoral sheath is usually placed in the artery through which different catheters or guide-wires can be inserted.
The abdominal aorta with its various branches is visualized. Then a very small catheter (micro catheter) is passed through the liver artery into the artery supplying the tumor and the chemoembolization is performed.
The patients are given pain medications through infusion to prevent pain during the procedure.
The chemoembolization agent are usually composed of:
Mitomycin C or Gemcitabine or both combined (chemotherapeutic) in combination with Lipiodol and Spherex (blocks blood vessels).
The sensitivity of the liver tumor (chemosensitivity) to a particular chemotherapeutic agent can be tested before the procedure through a biopsy from the targeted liver lesion which helps to achieve better results with the mentioned treatment procedure.
At the end of transarterial chemoembolization and after removal of the catheters and femoral sheath, a pressure bandage is applied to prevent any complications in the inguinal region (e.g., haematoma). The patient is then placed for observation for about 6 hours during which possible complications can be diagnosed and treated.
To evaluate the success of the treatment and to rule out a complication, the patient undergoes a check MRI on the same day of chemoembolisation and likewise a CT follow-up on the following day without contrast agent.
Typically the chemoembolisation is done in 2-3 cycles at an internal of 4 weeks between the cycles but some cases may require more cycles depending on treatment success.
3D imaging of the hepatic arteries with the special robot Artis Zeego
Graphic representation of TACE therapy in the liver
Source: Prof. Dr. med. Nagy Naguib, Size: 9,1 MB , Duration: 01:43 min
Side effects
Postembolisation syndrome (PES) with nausea, vomiting, abdominal pain and fever can occur in 10% to 90% of TACE cycles according to our experience, but depends on the selective technique and the volume of cytostatic and embolic agent. According to our own data, the frequency of PES is 3-5%. The aetiology of PES is not fully understood; it is most likely the combination of tissue ischaemia and an inflammatory effect of chemoembolisation.
effect of chemoembolisation. The development of PES affects the post-interventional procedure and often necessitates hospitalisation. Rates of relevant complications after TACE range from 2% to 7% depending on the technique and experience of the interventional team. TACE is performed at many centres as an outpatient or inpatient procedure. The frequency of PES in patients receiving embolisation plus chemotherapy (TACE) is similar in frequency and intensity to the patient population receiving embolisation alone. It can be concluded that the ischaemic effects are predominant in hepatic chemoembolisation. The factors that may influence the manifestation of PES are inadvertent embolisation of vessels to the gallbladder, tumour size, embolised healthy liver area, number of previous TACE cycles and dose of chemotherapy. A reduced rate of PES is often observed with repetitive TACE. One of the most serious complications of TACE is hepatic dysfunction, including liver failure; in the majority of cases, the deterioration in liver function lasts
less than one week and is reversible. Chan et al. prospectively analysed the risk factors that favour the development of acute irreversible liver failure after TACE: These are a high amount of cytostatic drugs (including cisplatin), an initially high serum bilirubin > 2.5 mg/dl, a reduced Quick value and advanced liver cirrhosis. When these values were taken into account, irreversible liver failure was found in only 3% of patients with TACE. However, in this
group, however, the survival rates of patients are significantly reduced compared to patients without irreversible hepatic failure.
Testimonials from patients
Dear Prof. Dr. Vogel,
Yesterday evening, after the first embolisation session, I drove home very euphoric and with a deep feeling of satisfaction that I had made the right decision in a very important life situation for me. Why?
In thorough discussions with 5 chief surgeons of German liver centres, it was made clear to me that open surgery to remove my 3-4 liver metastases was the right way to go, not least because of my portal vein thrombosis. Systemic treatment was certainly also an option, but was too risky for me because of the biopsy. Then your phone call reached me in the car at about 9 pm. I had contacted you by e-mail. You told me crisply and precisely that you could solve the problem much more gently at my age (77 years) with a combination of embolisation and ablation. Oops, that was a sign from God. But serious? Oops, an internet search quickly made it clear to me that I had the chance to get my liver problem under control in a gentle but very effective way with one of the world's best and most experienced radiologists. Boom, that was it. An appointment was quickly found and after the first session I feel happy and urged to write you these lines. Because what did I experience yesterday?
First 1.5 hours of annoying waiting time but then a professor who radiated so much calmness, composure, empathy, interest that you couldn't help but think, in whose hands you are in safe hands. And with technical equipment that is second to none. A pimped Tesla 3 MRT from Siemens, the highest resolution X-ray machine and the professor's sure hand for the various cannulas and medicines. Could there have been any other choice for me? Definitely a huge NO.
Now I am sitting on the sunny terrace the next day, have regained my zest for life, did my 3.5 km walking round this morning without any problems, did not feel any serious pain in my groin, and have blocked out the little bit of heartburn and stomach rumbling and dispensed with the medication given to me. I even drank a bottle of Altbier and a glass of rosé with my wife last night after returning home. What more do I want?
But one more thing. A thank you also to your fellow campaigners. An excellent leadership culture, exemplified by you, can be felt here. What you have imparted to me personally in this short time, you also pass on to your staff every day. And that, along with the technical equipment, is an indispensable asset for your excellent work. You know how to take patients and staff along with you in a reliable, competent way, which creates great trust. Therefore, at the end, a greeting to your secretary Mrs. Ossmann (she was the only one whose name we kept). We had a very funny farewell with her around 7:30 pm after the CT. So good-buy is still fun even at this level.
I am therefore looking forward with great confidence to the second appointment in 2.5 weeks with the certain hope that you will significantly improve your statistics with my treatment. I will do everything that you can take responsibility for and feel is right.
With gratitude and best regards
Technical papers and scientific studies on transarterial chemoembolisation (TACE)