Percutaneous transluminal balloon angioplasty (PTA) is a minimal invasive therapy option for the treatment of peripheral vascular diseases (PVD) or peripheral arterial diseases (PAD) in addition to other conservative therapies, lysis and vascular surgery. With significant development of catheter technology in the last decade it is possible to even perform extraction procedures today, especially procedures like Rotablation and ELA are being increasingly gaining prominence. Despite the impressive initial success rate of PTA, it has to two major disadvantages: firstly it is associated with a high restenosis rate which lies at about 50-60% and secondly it is only possible to treat the lesions that are accessible by the guide wire. Hence the performance of PTA is limited to stenoses or occlusions measuring less than 5 cm in length. In occlusions longer than 5 cm, the lone performance of PTA is not frequently successful. Such cases present the indication for performance of "Debulking" like the Excimer Laser-assisted Angioplasty.
Vascular Interventions
Excimer laser-assisted angioplasty (ELA)
Ablation of vaso-occlusive material by laser beams.
Excimer laser-assisted angioplasty for peripheral arterial disease (PAVD)
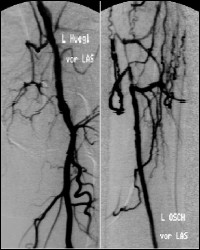

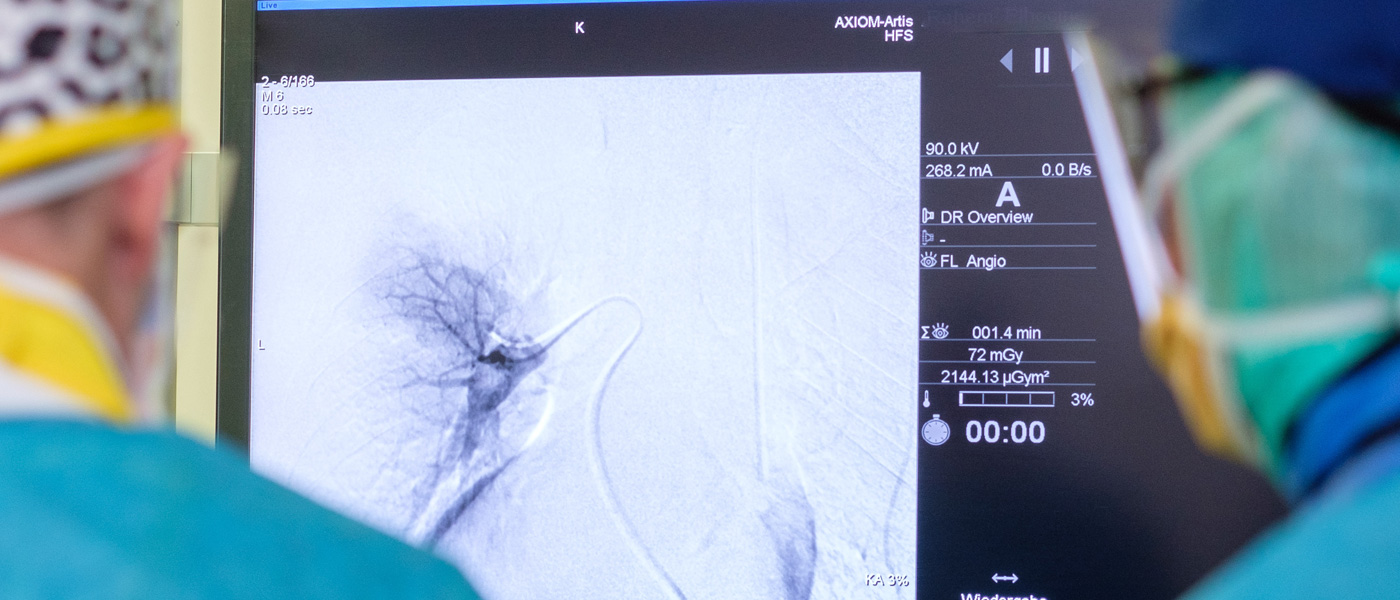
Figure 1a: A 48-years-old patient with grade IIb PVD since 18 months, digital subtraction angiography shows a long segment stenosis of left superficial femoral artery.
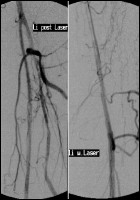
Figure 1b: Follow-up DSA after recanalisation of the long segment occlusion of left superficial femoral artery with a 2,5 multiphase catheter. The follow-up angiography shows a now patent vascular lumen but still with evidence of restenoses and a dissection.

Figure 1c: Finally a follow-up DSA after supplementary PTA shows a complete reperfusion of supercial femoral artery without residual, hemodynamic relevant restenosis or dissection.
Principle of Excimer Laser-assisted Angioplasty
Principally the laser-tissue interaction is due to the absorption of photons and the duration of laser application. Thus, the absorbed (deposited) photon energy is converted to another form of energy in the tissues (for e.g., thermal, chemical and mechanical energy). The depth of tissue penetration by the laser is determined or dependent on different wave lengths of the laser. The main thermal changes caused are coagulation and vaporisation of the tissues. The photothermal changes are mostly brought about by the use of Nd:YAG and Argon Laser. Photoablation and photodisruption (optical penetration) are grouped into photoionising and oligothermal changes which is characterized by application of high density rays for a very short affection time (laser pulse in nsec likewise in µsec). The photoablative change is achieved by the pulsed Excimer-Laser. The photoablation leads to rapid necrosis of the target tissue with minimal thermal effect of the surrounding tissues. Hence, the necrosed zone of the surrounding tissue is less than 50 µm whereas the thermal necrosis of the target zone is more than 50 µm.
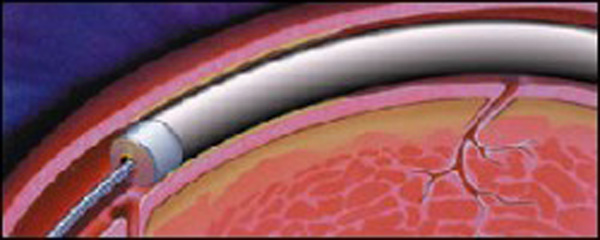
Placement of the balloon catheter within the artery.
Dilatation of the balloon catheter within the artery.
Patent artery after balloon dilatation.
Excimer laser-assisted angioplasty technique
In principle, laser-tissue interaction is based on the absorption of photons and the duration of application. In the process, the absorbed (deposited) energy of the photons is converted into other forms of energy (e.g. thermal, chemical or mechanical energy) in the tissue. Depending on the different wavelengths of the laser radiation, different penetration depths are found when soft tissue is irradiated. The main thermal effects of laser radiation are coagulation and vaporisation of tissue. The most important representatives for photothermal interactions are the Nd:YAG and argon lasers. The group of photoionising, oligothermal effects includes the photoablative and photodisruptive effects (optical breakdown), which are characterised by high power densities at very short exposure times (laser pulses in the ns or µs range). Photoablative interactions can be achieved with the pulsed excimer laser. Athermal is defined by the size of the thermally damaged marginal zone. In photoablation, the ablation of the irradiated tissue occurs explosively at several times the speed of sound, with low thermal stress for the surrounding, non-irradiated tissue. The damage zone of the surrounding tissue is <50 µm, whereas in thermal tissue ablation the damage zones are >50 µm.
1. Patient Consent.
The consent should be taken a day before at the least.
Patient consent on day of therapy only in case of emergencies.
In children below 16 years of age, a written consent of the parents or guardians and when possible signature of both should be obtained.
In case of unconscious emergency patients, a written understanding between the treating doctor and radiologist should be obtained.
Associated Disease.
|
Hyperthyrosis, Goitre |
Serum TSH level, prophylaxis with Irenat |
|---|---|
|
Renal insuffifiency |
Creatinine > 1,5mg/dl Creatinine 1-1,5 mg/dl; Patient should be hydrated properly Creatinine > 2 mg/dl: Nephrological consultation for haemodialysis after angiography |
Interaction with Medications
|
Marcumar or Warfarin |
Stop intake a week before procedure. Substitute with Fraxiparin. Check Quick level! |
|---|---|
|
Glucophage or Metformin |
Stop intake 2 days before procedure. |
|
Allergy to contrast media |
Premedication with Cortisone, H1 and H2 blockers. |
Blood Parameters
Blood parameters should not be older than 2 weeks (TSH 4 weeks).
Report should contain:
Thrombocyte count, creatinine levels, eventually TSH.
For patients under warfarin or heparin therapy: Quick, PTT and INR.
For Chemoembolisation of liver additional hepatic enzyme, bilirubin and CHE.
On the Day of Examination or Intervention
Preparation for ELA
Fasting:
The patient should not eat, drink or smoke 6 hours before the examination.
Oral medications and insulin can be taken after consultation with the treating physician.
Patient education
For planned procedures, at the latest the day before.
Patient information before the start of the examination only in case of emergency indication.
In the case of children under 16 years of age, the written consent of both legal guardians or one legal guardian who signs for both, if necessary, applies.
In the case of unconscious emergency patients, the principle of presumed consent can be applied; in this case, the written consent of the referring doctor applies as a substitute.
Inclusion criteria for the ELA

ELA is indicated for patients with stage II to IV PAVD according to FONTAINE. Patients with claudication lasting longer than six months and a reduced walking distance of between 200 and 500m can also be treated with ELA if their quality of life is significantly reduced. In particular, patients with single or multiple, subtotal or total stenoses in the iliac artery, femoral artery or popliteal artery can be treated with ELA, provided that connecting vessels with sufficient blood flow are available. Experience in recent years has shown that even occlusions > 20 cm can be successfully recanalised with ELA. The indication for ELA should be made on the basis of a technically perfect, up-to-date DSA.
Success rate
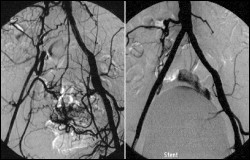
Arterial occlusion before and after laser treatment
With ELA of the pelvic region, successful recanalisation is achieved in 94.3%. The recanalisation rate drops to 78% for occlusion lengths between 3 and 7cm. Successful laser recanalisation with a 7F or 9F laser catheter is followed by localised conventional PTA. In addition, there is often an indication for stent implantation, especially if there is evidence of residual stenosis of >50%, and intervention-related dissections. Careful intervention planning using CT angiography of the pelvic vessels is essential pre-intervention. With this technique, the exact course of the vessel as well as the degree and localisation of calcifications can be documented.↵
Superficial femoral artery: For subtotal stenoses or occlusions up to approx. 3 cm in length, a primary success rate of 95% can be achieved. For occlusion lengths between 3 and 7cm, the primary success rate is > 90%. The primary success rate drops to about 76% for occlusion lengths between 7 and 12 cm. In the majority of cases, primary unsuccessful recanalisation in these groups is due to failure to reach the distal reconnection segment. Consecutively, a further decrease in the primary success rate to 71% can be observed for occlusion lengths of the superficial femoral artery between 12 and 42 cm. After successful laser recanalisation, a targeted PTA of remaining stenoses is performed. This can significantly reduce the likelihood of dilatation-related vessel dissection.↵
Popliteal artery: ELA in the popliteal artery, including the trifurcation, is technically possible, but has a low primary success rate of approximately 72% due to the involvement of the lower leg vessels associated with PAVK. Our previous experience in this section of the vessel showed that a so-called "stand-alone" laser recanalisation with a 6F or 7F multifibre catheter is to be preferred and should not be supplemented by a combined balloon angioplasty. Due to the relatively small number of patients in this vascular group, a conclusive statement on the value of "stand-alone" laser recanalisation cannot be made at present.