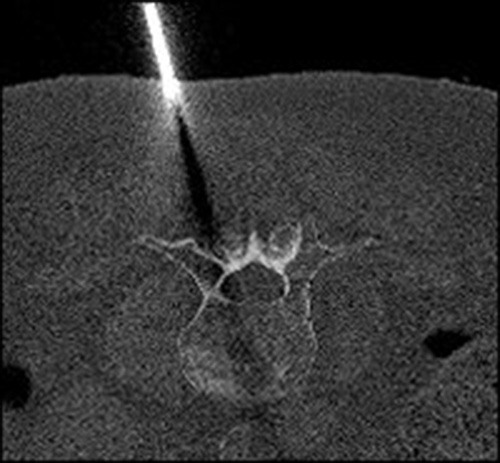
CT control of the position of the puncture needle
Vertebroplasty / Osteoplasty
Co-operation between the Institute of Diagnostic and Interventional Radiology (Johann Wolfgang Goethe University Hospital), Department of Accidental, Hand and Reconstructive Surgery (Johann Wolfgang Goethe University Hospital) and Department of General Orthopaedics and Traumatology (Orthopaedic University Hospital, Friedrichsheim).
Dear Patients,
In the following pages we would like to inform you about the various interventional therapies for pain reduction und stabilisation of vertebral body fractures through percutaneous application of bone-cement in patients with osteoporosis and malignant bone tumors.
The percutaneous vertebroplasty / osteoplasty is an effective new interventional-radiological therapy for augmentation of benign and malignant bone lesions with bone-cement (polymethylacrylate, PMMA) under the guidance of computer tomography and floroscopy. Through this method, which is already being performed successfully in France and the USA, it is possible to stabilize the diseased vertebra and thus achieve a significant reduction in pain.
The application of bone-cement has established itself as an endoprosthetic. Long-term studies have shown that with stable placement of bone-cement the normal bone substance remains vital for a long time. Filling of vertebral bodies with bone-cement as therapeutic method in oncological surgery and as percutaneous interventional method have been reported [Weill 1996, Jensen 1997]. A significant stabilization of vertebral bodies with malignant or benign lesions with interventional vertebroplasty has been proven [Gangi 1995, Deramond 1996, 1998, Cotton 1996, 1998, Cortet 1996, Martin 1999].
Intervention / Method
The intervention is performed under local anaesthesia mostly in combination with a neuroleptoanalgesia. The diseased vertebral body is reached with a special application set (needle) under the accurate step-by-step guidance of computer tomography and fluoroscopy. When the needle has been placed in diseased bone (pathological fracture or bone tumor), a special bone cement with minimum viscosity is injected through this needle under continuous fluoroscopic guidance. During the procedure the patient is constantly observed and checked for blood pressure, oxygenation (PO2) and pain symptoms. The procedure lasts about 50 - 60 minutes. After the application of the bone cement the patient is placed on observation for about another 6 hours. Following a complication-free observation period the patient is discharged. After the vertebroplasty there can be an increase in pain symptoms for a few days. In most of the cases there is significant reduction in pain after 24 hours which will last for weeks up to months.
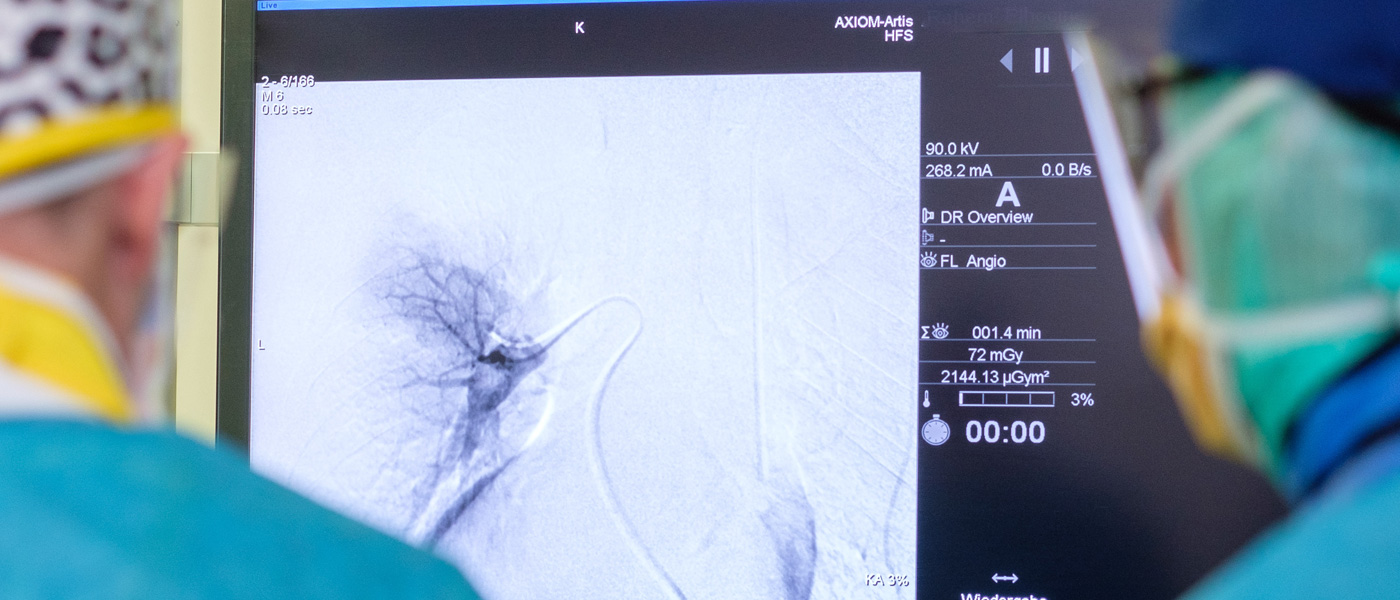
Performance of Vertebroplasty under fluoroscopy and CT guidance.

Application of the bone cement under fluoroscopy
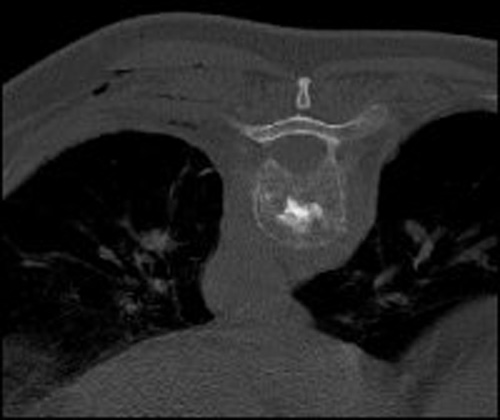
CT check after application of the bone cement
- Percutaneous vertebroplasty:
- Injection of 3.5 ml bone cement
- Transpedicular route
- Indication: vertebral body fracture
Local anaesthesia under CT control
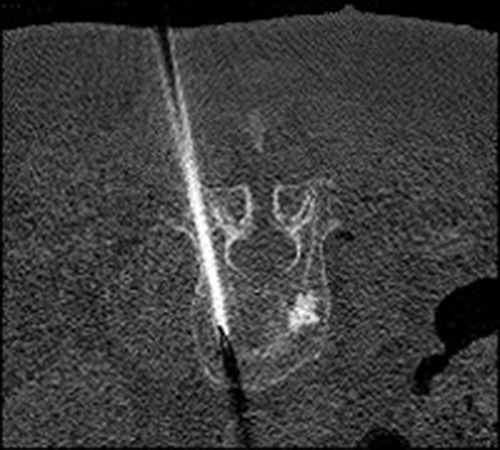
Puncture under CT-control
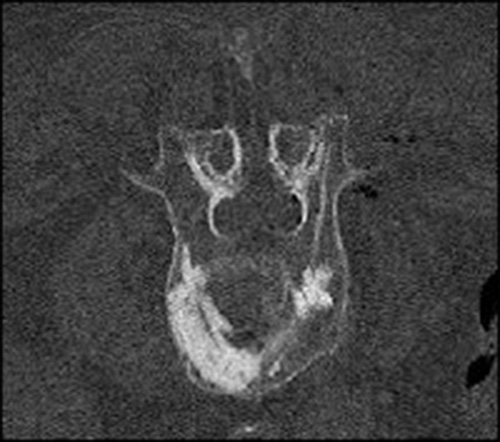
After application of the cement CT control
What is osteoporosis?
Osteoporosis is a metabolic disorder of the bones which causes loss of the bone substance, change in its micro architecture and leads to loss of stability and fracture. These fractures mostly occur in the thoracic and lumbar vertebra. Females above 50 years of age have an increased life time risk of fractures: 15.6% in vertebra, 17.5% in hips (femur) and 39.7% elsewhere. The consequences are decrease in height, kyphosis (Gibbus) and reduction in distance between ribcage and pelvis. Once these changes have occurred , they are irreversible. Patients with fresh vertebra fractures have severe debilitating pain leading to significant disability which sometimes could be very extreme. Medical therapy for stabilization of other vertebra can be tried but this is relatively of little help in terms of biomechanical stability. Moreover the yearly increase in bony substance with medical therapy is only marginal. Hence there are chances of new fractures in other vertebra. Operative treatment of osteoporotic fractures are problematic because the decreased bone density and stability of other vertebra frequently doesn't allow an adequate fixation with osteosynthesis.
Spinal fractures with bone metastases
With the documentation of a bony metastases is the tumor thought to be in a generalization stage. No matter what therapy is undertaken at this stage it is only palliative. The main objective of percutaneous vertebroplasty, also a palliative treatment, is reduction in pain symptoms, restore functionality (stabilization of fracture) likewise maintenance of function (prevention of fracture) and improvement in quality of life. With radiation therapy the achievement of reduction in pain is only gradual over a period of time, the aimed consolidation of bone is only partial and takes weeks to months.
The decision of performance of percutaneous bone augmentation (vertebroplasty) should be multidisciplinary with involvement of radiologists, surgeons or orthopaedic surgeons, radiotherapists and medical oncologists. The therapy depends on the primary illness, the local and general extension of the illness, infiltration of nearby structures, neurological symptoms, pain symptoms and life expectancy. In some cases a combination of different therapeutic modalities is needed because vertebroplasty is not a tumor-specific therapy substitute but only a therapy supplement.