Prostatic-Embolization for Benign Prostatic Hyperplasia
Special minimal invasive Therapy for Benign Prostatic Hyperplasia
What is benign prostatic hyperplasia?
Benign non-cancerous enlargement of the prostatic gland due to an increase in the amount of prostatic tissue.
Is it common to have benign prostatic hyperplasia
Up to 70% of men above 60 years suffer from symptomatic benign prostatic hyperplasia.
What symptoms does benign prostatic hyperplasia cause?
The urethra (urinary bladder outlet canal) passes through the center of the prostate. Enlargement of the prostate will result in stenosis of the urethra and difficulty in urinary bladder emptying. Patients with benign prostatic hyperplasia will suffer from lower urinary tract symptoms. These include feeling of incomplete emptying of the urinary bladder, frequency (increased number of micturition times per day), weak stream of urine during micturition, intermittency (the need to stop and resume micturition), urgency (the need to immediately start micturition)
and nocturia (the need to urinate several times at night).
- the feeling of incomplete emptying of the bladder
- frequent urge to urinate
- weak urine flow
- interruption and continuation of micturition
- Tightness during micturition; and
- nocturia (nocturnal bladder weakness).
What are the treatment options?
Depending on the degree of symptoms and the doctor's and patient's preference, there are several therapeutic options. Drug therapy can lead to a significant improvement in symptoms. If the drug option fails, there are numerous surgical options. The gold standard method is transurethral resection of the prostate (TURP). Retrograde ejaculation (flow of semen when ejaculating into the bladder instead of through the urethra), bleeding, stress incontinence, urethral stricture and reintervention are possible complications of TURP. The minimally invasive treatment option (prostate embolisation) offers an alternative to surgery.
What is prostate embolisation and who performs it?
The choice of treatment reflects the severity of symptoms and preferences of patient and physician. Medical treatments
aiming at improvement of patient symptoms are widely used and result in marked improvement of symptoms. For patients who do not respond to medical treatment several surgical and endoscopic procedures are available. The most commonly used method of treatment is transurethral resection of the prostate (TURP). This method is considered the gold standard treatment method for benign prostatic hyperplasia. Retrograde ejaculation (passing of seminal fluid into the urinary bladder during ejaculation), bleeding, stress incontinence, urethral stricture and need for resurgery are among the possible complications of TURP. Several other alternatives are available including angiographic techniques (prostatic artery embolization).
What is prostatic artery embolization and who performs it?
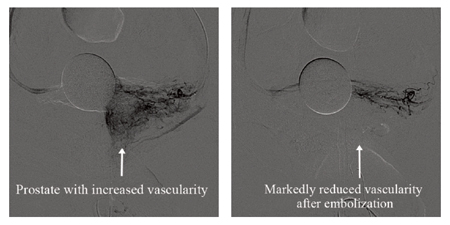
The prostatic artery is the artery carrying blood to the prostate and embolization means injection of a substance to block blood vessels and stop the blood flow. This procedure has been successfully used for over 20 years to control various causes of bleeding (e.g. uncontrolled bleeding due to prostatic cancer). Its use in treatment for benign prostatic hyperplasia started in the year 2008 (animal trial) and 2010 where the first human cases were performed. It is performed by physicians specialized in the field of interventional radiology.
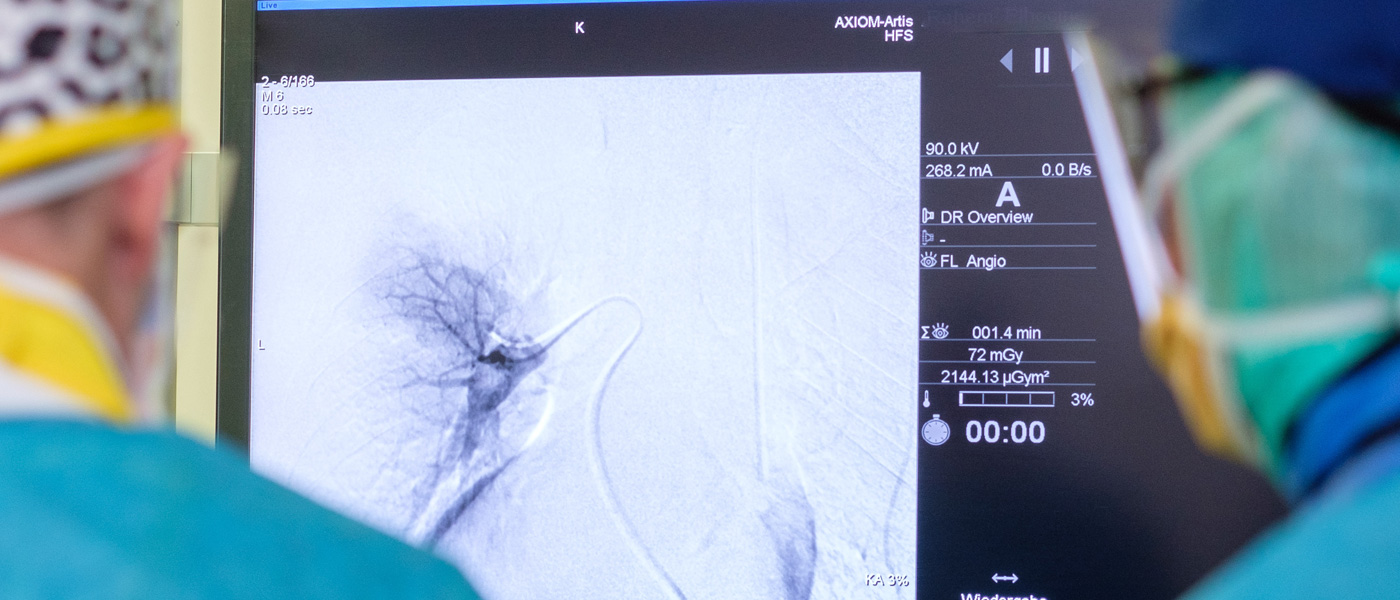
How is it done?
The procedure is done under imaging guidance. First a local anaesthesia is injected in the groin (usually the right side). Then a small opening is made in the artery (about the size ofa needle diameter). Through this opening a catheter is introduced (a thin flexible special tube) and manipulated under angiographic guidance till the prostatic artery is reached. Then the embolizing material (which are very small particles) is
injected into the prostatic artery on each side. In Frankfurt we developed a new technique to markedly reduce the amount of radiation use during pelvic interventions. This technique depends on planning the procedure using magnetic resonance imaging before the procedure. This leads to a marked reduction of the radiation exposure and a reduction in the volume of the used contrast medium.
How long do I need to stay in the hospital?
The procedure can be done on an outpatient basis. Usually you can resume your normal activity within few days after the procedure.
What is the incidence of complications?
Some of the complications are related to the interventional procedure itself, e.g. hematoma formation at the puncture site. Other complications are related to the prostate embolization including possible bleeding on urination or defecation, infection of the prostate, bleeding with semen. All of these complications are temporary and resolve spontaneously. Severe complications requiring surgical intervention include bladder wall ischemia occurring in less than 1% of cases.
Complications like impotence, retrograde ejaculation and incontinence related to the embolization have not yet been reported in the medical literature.
How successful is it?
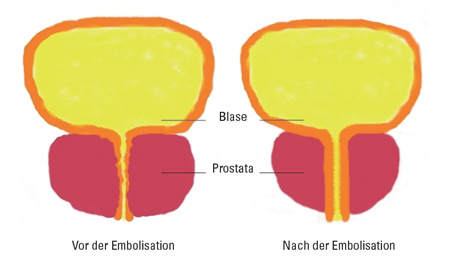
The reduced blood supply to the prostate will help shrinking the size of the gland with subsequent improvement of the lower urinary tract symptoms and reduction of the compression of the urinary bladder outflow tract. A recently published review of the literature published in 2014 by Schreuder et al. showed marked improvement of the symptoms. They showed an improvement of the patient’s severity of symptoms from a score of 23.31 to a score of 8.1 after 30 months. In addition the impact of urinary symptoms on the quality of life improved from a score of 4.34 to a score of 1.85 after 30 months.
Further information and details
Further information and details
Team
Prof. Dr. med. Thomas J. Vogl
Tel.: (069) 6301-7277
Fax: (069) 6301-7288
E-Mail: t.vogl@em.uni-frankfurt.de