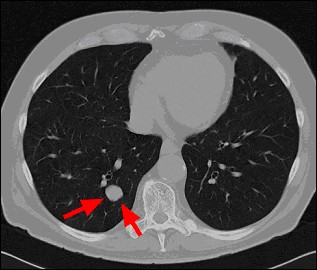
Small bronchial carcinoma located at the periphery without evidence of mediastinal lymph nodes (T1N0M0).
Bronchial carcinoma
Information about the Development, Diagnosis, Treatment
Dear Patients,
On this page we would like to inform about the possibility of onco-CT at our institute.
Bronchial Carcinoma / Lung Cancer
Facts:
About 54000 deaths in a year in Germany are due to bronchial carcinoma (lung cancer) - about 29000 men and 25000 women). Hence like in the rest of the world bronchial carcinoma is the most common cause of cancer deaths in Germany.
About 40% of patients have a life expectancy of 5 years after diagnosis of bronchial carcinoma.
Risk Factors:¶
1st risk factor: smoker
2nd risk factor: occupational exposure of carcinogenic substances.
Data:
Active smoker: 12 - 22 times increased risk of developing bronchial carcinoma (when compared to non-smoker)
Various substances in smoke of tobacco damage the cells of the bronchial system which over the years lead to conversion of normals cells into cancerous cells.
Normally the human body through its immune system recognises the cancer cells and eliminates them. When the tumor cells succeed in overcoming the immune system, it leads to constant differentiation which results in development of tumor nodules, proliferation and spread (metastases) to other regions of the body.
Survival chances and risks:
Scientific studies show that the earlier the diagnosis and treatment of lung cancer the better the survival chances.
The 5-year survival rate lies between 70-80% for tumors diagnosed and treated in their early stages.
Clue:
Measures to prevent occurance of cancer as well as early diagnosis lead to better survival rates.
Methods for early diagnosis of bronchial carcinoma (lung cancer):
Basically there are many radiological examinations for early diagnosis of lung tumors.
Up till now the diagnosis was focused on chest x-ray (bronchial system, cardiac system)
A further simple method of examination is the examination of sputum (bronchial mucous) for tumor cells but this technique is not suitable for early cancer diagnosis so that it could improve the survival rate.
Oncology oriented computer tomography (CT) of the chest can in comparison to other modalities detect tumors as small as 2-3 mm. When tumors are detected at this phase it is called a very early stage, the so called stage 1A.
According to the Early Lung Cancer Action Programme (ELCAP), a study from Cornell University New York, it has been shown that CT is capable of detecting most of the tumor nodules in very early stage, in stage 1A.
This brings with it the advantage of increasing the 5 year survival rate upto 70 - 80%. Hence CT of the chest is the method of choice for early detection of lung tumors.
A few characteristics of Onco-CT (Lungs)
- Computer tomography performed specially with low radiation dose (low dose CT).
- The examination is performed in a very modern machine (multislice computer tomography).
- Data processing: 4-8 seconds.
- Radiation dose: Similar to conventional chest x-ray in two projections.
- Spatial resolution: it is 10 to 100 times compared to chest x-ray
- Interval of follow-up examinations:
- Active smoker: yearly follow-up.
- Definition of an active smoker: packs/year (packs/year x years) which means 1 pack per day for 10 years or 2 packs per day for 5 years.
- In case of ex-smokers follow-up should be done regularly for the first 10 years after nicotine abstinence.
- After a time interval of 10 years the risk of developing lung cancer (or bronchial carcinoma) equals that of normal non-smoker population.
"What next" after detection of a suspicious lung nodule in Onco-CT. Following situation:
1. The Onco-CT shows normal findings: this means that the probability of bronchial carcinoma is extremely small. Exception: a tumor process in the mucous membrane of bronchial system.
2. The Onco-CT a calcified/multiple calcified nodules (granulomas): This is suggestive of a past lung infection or tuberculosis.
3. The Onco-CT shows non-calcified nodules:
Nodule > 4 mm non-calcified: a 6 monthly follow-up examination is suggested. If the nodule remains constant in size and density in follow-up examination then it is most probably a benign lesion.
4. The Onco-CT shows a calcified nodule:
The nodule increases in size: this is suggestive of malignancy and a further confirmatory examination suggested. This is usually CT-guided biopsy for histological examination.
Nodule < 4 mm: A follow-up is suggested in this case too at 6 months interval.
Increase in size:
In case there is an increase in size of the nodule, a histological confirmation should be done. Should the nodule be histologically positive for cancer it should be operatively removed.

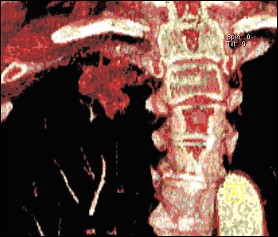
Three dimensional visualisation of a peripherally located bronchial carcinoma at tip of right lung (Overview).
Thee dimensional visualisation of peripherally located bronchial carcinoma at tip of right lung (coned down view).