
Klinik für Radiologie und Nuklearmedizin am Universitätsklinikum Frankfurt
Unsere Klinik zählt zu den modernsten radiologischen Kliniken in Deutschland und ist zentraler Bestandteil des Universitätsklinikums Frankfurt am Main. Gemäß dem Grundsatz des Klinikums "AUS WISSEN WIRD GESUNDHEIT" versorgt unser Team alle Patienten auf höchstem wissenschaftlichem Niveau der modernen Radiologie. Dabei kommen High-End bildgebende diagnostische und minimalinvasive Verfahren zum Einsatz.
Gemäß unseren Leitlinien spielen auch die Forschung und Lehre eine besonders große Rolle an unserem Institut. Da sich die klinische Diagnostik und interventionelle Therapie sowie die Forschung und Lehre in verschiedene Fachzentren unterteilen, dürfen wir Sie einladen, sich auf diesen Seiten über alle Bereiche unserer Klinik zu informieren.
Schwerpunkte der Klinik
Diagnostische Radiologie
Interventionelle Radiologie
Fachbereiche
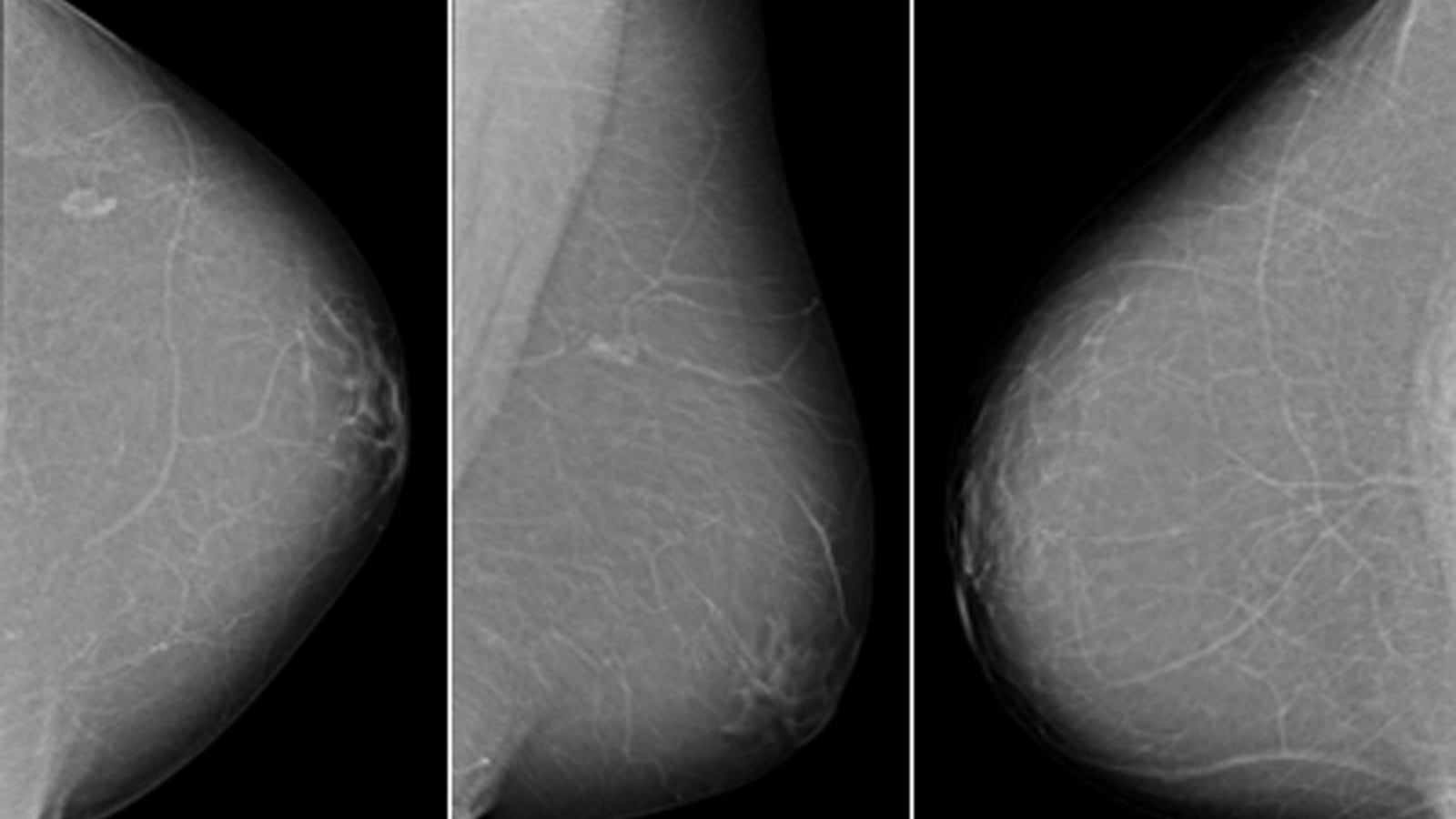
Gynäkologische Radiologie
Die Gynäkologische Radiologie beschäftigt sich mit Erkrankungen der Brust (Senologie). Sie ist ein Teilbereich des Instituts für Diagnostische und Interventionelle Radiologie.
Kinder- und Jugendradiologie
Spezielle Radiologen für die Kinder! Kinder sind keine kleinen Erwachsene. Die bildgebende Diagnostik ist das zentrale Aufgabengebiet unserer Kinder- und Jugendradiologie.
Veranstaltungen
Aktuelles und Forschung
HERR HAMZAH ADWAN BEKAMM BEIM 4. IMSCB DEN ZWEITEN PREIS VERLIEHEN
Nominierung für den German Medical Award 2020 in der Kategorie "Innovation - Verfahren für Praxen und Kliniken"
Prof. Dr. Thomas J. Vogl ist Kongresspräsident des 102. Deutschen Röntgenkogresses
Dr. Martin ist ein Top-Gutachter des European Journal of Radiology 2019
Veröffentlichungen
Podcast von Prof. Vogl "Interventionelle Therapie bei Tumoren und Metastasen an Lunge
Video Tatort Radiologie: Mord am Mainufer mit 'Sherlock Vogl'
Ihre Karrierechance bei uns
Wir freuen uns jederzeit über Ihre Bewerbung als:
Assistenzärztin / Assistenzarzt in fortgeschrittener Facharztausbildung für Diagnostische Radiologie mit Schwerpunkt Onkologische Bildgebung und Onkologische Interventionen als Advanced Clinician Scientist
oder
Fachärztin / Facharzt für Diagnostische Radiologie mit Schwerpunkt Onkologische Bildgebung und Onkologische Interventionen als Advanced Clinician Scientist
oder
Fachärztin / Facharzt für Diagnostische Radiologie mit Schwerpunkt Onkologische Bildgebung und Onkologische Interventionen als Advanced Clinician Scientist
Medizinisch-Technische Radiologieassistentin
Medizinisch-Technischer Radiologieassistent
Medizinisch-Technischer Radiologieassistent
Mitgliedschaften & Auszeichnungen
-
PRIMO MEDICO Netzwerk
Herrn Professor Thomas J. Vogl wurde durch Asmus Grebbin, Geschäftsführer von PRIMO MEDICO, das Siegel des Jahres 2018 überreicht. Dadurch ist Professor Vogl offizielles Mitglied des Netzwerkes mit bislang über hundert medizinischen Spezialisten unterschiedlicher Fachbereiche aus Deutschland, Österreich und der Schweiz.
Geräteausstattung
Kontakt
Vereinbaren Sie Ihren Untersuchungstermin von Montag bis Freitag in der Zeit von 07:30 bis 17:00 Uhr.
Sekretariat Prof. Thomas J. Vogl
069 6301-7277
Interventionsambulanz
069 6301-4736
Zentral-Radiologie
069 6301-87202
Gynäkologische Radiologie
069 6301-5174
Kinder- und Jugendradiologie
069 6301-5248







